More Evidence Showing Vitamin D Combats Cancer
All Global Research articles can be read in 51 languages by activating the Translate Website button below the author’s name (only available in desktop version).
To receive Global Research’s Daily Newsletter (selected articles), click here.
Click the share button above to email/forward this article to your friends and colleagues. Follow us on Instagram and Twitter and subscribe to our Telegram Channel. Feel free to repost and share widely Global Research articles.
Global Research Referral Drive: Our Readers Are Our Lifeline
***
Evidence continues to accumulate showing that vitamin D is a strong ally to combat cancer
Low vitamin D levels are linked to an increased risk of cancers, while vitamin D can attach to the vitamin D receptor (VDR) in your cells, setting off a series of signals that may affect how they grow, develop and survive
Although increasing vitamin D levels may help to reduce cancer deaths, health officials rarely recommend optimizing levels for this purpose
Vitamin D targets cancer in multiple ways, including anticancer, antimetastatic and anti-tumorigenic effects
The best way to optimize your vitamin D level is via regular sun exposure, which enhances production of melatonin — a potent anticancer agent
*
I strongly recommend getting sensible sun exposure each day, and one of the reasons why is because it helps naturally optimize your vitamin D levels. Low vitamin D levels are linked to an increased risk of cancers,1 while vitamin D can attach to the vitamin D receptor (VDR) in your cells, setting off a series of signals that may affect how they grow, develop and survive.2
In this way, vitamin D acts like a brake on the process of cell growth in many tissues of the body, helping to control the speed at which cells multiply. This is particularly important when it comes to cancer because one of the key features of this disease is cells growing out of control. Moreover, vitamin D has been observed in animal studies to help delay some age-related changes by activating another important pathway via the vitamin D receptor.
This pathway involves a molecule called Nrf2, which plays a crucial role in protecting your body from oxidative stress and DNA damage — two factors that are commonly linked to the development of cancer.3 Overall, evidence continues to accumulate showing that vitamin D is a strong ally to combat cancer.4
Vitamin D Reduces Cancer Mortality
Worldwide, cancer is the no. 2 cause of death, behind only cardiovascular disease.5 Meanwhile, the global prevalence of vitamin D deficiency (defined as a level of less than 20 ng/mL) and insufficiency (defined as a level of 20 to less than 30 ng/mL) is 40% to 100%.6 Although increasing vitamin D levels may help to reduce cancer deaths, health officials rarely recommend optimizing levels for this purpose.
For example, research has shown that once you reach a minimum serum vitamin D level of 40 ng/mL, your risk for cancer diminishes by 67%, compared to having a level of 20 ng/mL or less.7
A 2023 systematic review and meta-analysis published in Ageing Research Reviews also found vitamin D3 supplementation reduced cancer mortality by 6%. This wasn’t considered statistically significant, but when only studies involving daily vitamin D intake were analyzed, cancer mortality dropped by a significant 12%.8 According to the researchers:9
“From a biological perspective, it is plausible that a sufficient vitamin D status has an impact on cancer prognosis: by binding to the vitamin D receptor (VDR), the active hormone 1,25-dihydroxyvitamin D (1,25(OH)2D) influences signaling pathways that regulate cell proliferation, differentiation, and cell survival, and thus acts as an anti-proliferative agent in many tissues and can slow the growth of malignant cells.”
Other research also supports vitamin D’s role in protecting against cancer death. In one study of 25,871 patients, vitamin D supplementation was found to reduce the risk for metastatic cancer and death by 17%. The risk was reduced by as much as 38% among those who also maintained a healthy weight.10,11
What’s particularly noteworthy is this study only gave participants 2,000 IU of vitamin D daily and didn’t measure their blood levels. Despite these research flaws, a significant benefit was still found. However, other research has found even more striking benefits, including a GrassrootsHealth analysis published in PLOS ONE.
It showed women with a vitamin D level at or above 60 ng/mL (150 nmol/L) had an 82% lower risk of breast cancer compared to those with levels below 20 ng/mL (50 nmol/L).12 Meanwhile, risks of lung cancer, colorectal cancer, breast cancer, bladder cancer and lymphoma are higher in people with low vitamin D levels, while having higher levels is associated with a better prognosis in cases of breast and colorectal cancers.13
The Ageing Research Reviews study further revealed that daily vitamin D supplementation was particularly beneficial for people aged 70 and over, as well as those who took vitamin D daily and were later diagnosed with cancer. Study author Ben Schöttker, Ph.D., with the German Cancer Research Center in Heidelberg, further explained:14
“This does imply that basically everyone aged 50 and older, including people who have never had cancer, might profit from vitamin D supplementation if they are vitamin D insufficient … Doctors cannot know who might develop cancer at a later time.”
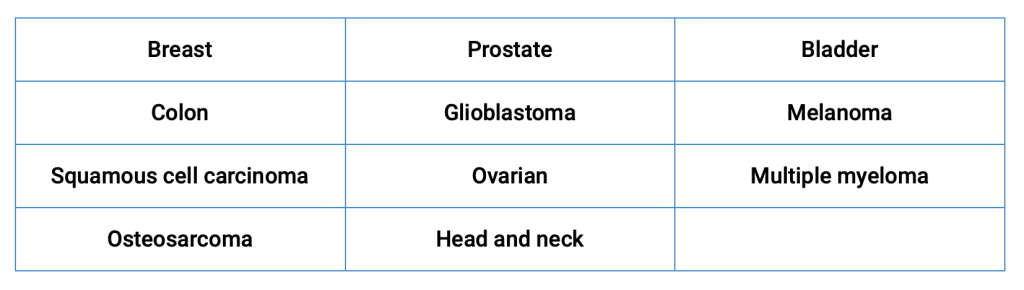
Vitamin D Has Anticancer Effects Against Many Types of Cancer
A mini review on the impact of vitamin D on cancer, published in The Journal of Steroid Biochemistry and Molecular Biology, pointed out that while vitamin D is widely recognized for its essential role in regulating the balance of minerals in the body, a deficiency has been linked to the onset and progression of various cancers.15 Vitamin D targets cancer in multiple ways, including:16
- Anticancer effects, which means it targets different stages of cancer development and progression, including the initiation, growth and spread of cancer cells.
- Antimetastatic effects, which refers to the ability to stop cancer cells from spreading from the original tumor site to other parts of the body. Since metastasis is often responsible for the fatal outcomes of cancers, preventing the spread can significantly improve survival rates.
- Anti-tumorigenic, meaning vitamin D helps prevent tumor formation or the growth of tumors. This can involve mechanisms like inducing cell death in cancer cells, blocking cell cycle progression, or inhibiting pathways that fuel tumor growth.
The review highlighted vitamin D’s role against the following cancers:17
In terms of breast cancer, the leading cause of death for women globally, vitamin D deficiency is common among patients, and those who are deficient are more likely to have more aggressive and harder-to-treat subtypes of breast cancer, such as higher grade and estrogen receptor-negative tumors.
The study also highlighted the role of genetic differences in the VDR that could influence breast cancer risk. In particular, in certain populations like North Indian women from New Delhi, variations in the VDR gene were identified as potential risk factors.18
In prostate cancer — the most common cancer in men — low levels of vitamin D were linked to high levels of dihydrotestosterone (DHT) in the prostate which is associated with the progression of prostate cancer.19 In addition, vitamin D may influence the activity of sirtuin 1 (SIRT1), which is known as a longevity protein. Optimizing your vitamin D levels may help boost your body’s natural cancer defenses, in part, via mechanisms involving SIRT1.20
Additional research suggests there may be considerable variation in how different individuals’ genes respond to vitamin D supplementation, which might explain why not everyone benefits equally from extra vitamin D.
For best results, the scientists suggest vitamin D supplementation should be personalized and “advocate for options tailored to individual vitamin D needs, combined with a comprehensive intervention that favors prevention through a healthy environment and responsible health behaviors.”21
Why Sun Exposure Is the Best Source of Vitamin D
On a typical sunny day, your body may produce up to 25,000 international units (IU) of vitamin D,22although many people aren’t in the sun enough to optimize their vitamin D levels. However, I strongly recommend getting your vitamin D from proper sun exposure, if possible, as it provides benefits beyond vitamin D optimization.
Higher levels of vitamin D may even serve as a marker for healthy sun exposure, which in turn may be responsible for many of the health benefits, which include reduced risk of cancer and increased longevity, attributed to vitamin D. Regular sun exposure, for instance, enhances production of melatonin — a potent anticancer agent.23
Near-infrared rays from the sun penetrate deep into your body and activate cytochrome c oxidase, which in turn stimulates the production of melatonin inside your mitochondria. Your mitochondria produce ATP, the energy currency of your body. A byproduct of this ATP production is reactive oxidative species (ROS), which are responsible for oxidative stress.
Excessive amounts of ROS will damage the mitochondria, contributing to suboptimal health, inflammation and chronic health conditions such as diabetes, obesity and thrombosis (blood clots). But melatonin essentially mops up ROS that damage your mitochondria. So, by getting plenty of sun exposure during the day, your mitochondria will be bathed in melatonin, thereby reducing oxidative stress.24,25
If you’re unable to get adequate sun exposure each day, vitamin D supplementation may be necessary. Keep in mind that 20 ng/mL, which is often used as the cutoff for vitamin D deficiency, has repeatedly been shown to be grossly insufficient for good health and disease prevention, which means the true prevalence of people without optimal levels of vitamin D is even greater.
The only way to determine how much sun exposure is enough and/or how much vitamin D3 you need to take is to measure your vitamin D level, ideally twice a year. Once you’ve confirmed your vitamin D levels via testing, adjust your sun exposure and/or vitamin D3 supplementation accordingly. Then, remember to retest in three to four months to make sure you’ve reached your target level.
The Optimal Vitamin D Level for Cancer Prevention
The optimal level for health and disease prevention, including cancer prevention, is between 60 ng/mL and 80 ng/mL (150-200 nmol/L), while the cutoff for sufficiency appears to be around 40 ng/mL. In Europe, the measurements you’re looking for are 150 to 200 nmol/L and 100 nmol/L respectively.
It’s important to remember that calcium, vitamin D3, magnesium and vitamin K2 must be properly balanced for optimal overall health. Your best and safest bet is to simply eat more calcium-, magnesium- and vitamin K2-rich foods, along with sensible sun exposure.
However, if you find supplementation is necessary after a serum vitamin D test, also supplement with magnesium and vitamin K2 (MK-7) to ensure proper balance. You’ll also want to ensure you’re following an overall healthy lifestyle to reduce your cancer risk as much as possible. As researchers explained in Nutrients:26
“Vitamin D supplementation is not the magic pill that miraculously solves the cancer burden or that can replace a healthy lifestyle. It is necessary to foster a good environment and invigorate a healthy lifestyle, including a high-quality diet and physical activity. Both have been proven to confer health benefits in many diseases, including cancer, and are the best preventive measures available.”
*
Note to readers: Please click the share button above. Follow us on Instagram and Twitter and subscribe to our Telegram Channel. Feel free to repost and share widely Global Research articles.
Notes
1, 15, 16, 17, 18, 19 The Journal of Steroid Biochemistry and Molecular Biology July 2023, Volume 231, 106308
2, 3 Ageing Research Reviews June 2023, Volume 87, 101923, Introduction
4 Substack, Dr. William Makis, April 18, 2024
5 J Thorac Dis. 2017 Mar; 9(3): 448–451
6 Endocr Pract. 2021 May; 27(5): 484–493., Introduction
7 PLOS ONE 2016; 11 (4): e0152441
8, 9, 13 Ageing Research Reviews June 2023, Volume 87, 101923
10 JAMA Network Open 2020;3(11):e2025850
11 The Sentinel November 22, 2020
12 PLOS ONE June 15, 2015 (PDF)
14 Medical News Today May 17, 2023
20 Int. J. Mol. Sci. 2023, 24(7), 6154; doi: 10.3390/ijms24076154
21, 26 Nutrients 2022, 14(21), 4512; doi: 10.3390/nu14214512
23 Youtube, The Joe Cohen Show, Episode 1, October 25, 2022, 4:00
24 Physiology February 5, 2020 DOI: 10.1152/physiol.00034.2019
25 YouTube, MedCram, Sunlight: Optimize Health and Immunity January 21, 2022